Clip When a patient is admitted to the PACU what are the priority interventions the nurse performs ?
Kinh Nghiệm Hướng dẫn When a patient is admitted to the PACU what are the priority interventions the nurse performs 2022
Họ tên bố(mẹ) đang tìm kiếm từ khóa When a patient is admitted to the PACU what are the priority interventions the nurse performs được Cập Nhật vào lúc : 2022-09-09 09:30:08 . Với phương châm chia sẻ Kinh Nghiệm về trong nội dung bài viết một cách Chi Tiết 2022. Nếu sau khi tham khảo tài liệu vẫn ko hiểu thì hoàn toàn có thể lại phản hồi ở cuối bài để Admin lý giải và hướng dẫn lại nha.Chapter 5. Oxygen Therapy
Nội dung chính- Applying and Titrating Oxygen TherapyWhat are the priority nursing interventions for the patient while in the PACU?What is the priority initial nursing assessment in the PACU?What does a PACU nurse do?What is the main focus of care in post operative recovery room?
Hypoxemia or hypoxia is a medical emergency and should be treated promptly. Failure to initiate oxygen therapy can result in serious harm to the patient. The essence of oxygen therapy is to provide oxygen according to target saturation rate, and to monitor the saturation rate to keep it within target range. The target range (SaO2) for a normal adult is 92 – 98%. For patients with COPD, the target SaO2 range is 88 – 92% (Alberta Health Services, 2015; Kane, et al., 2013; Perry et al., 2014).
Although all medications require a prescription, oxygen therapy may be initiated without a physician’s order in emergency situations. Hypoxia is considered an emergency situation. Most hospitals have a protocol in place allowing health care providers to apply oxygen in emergency situations. The health care provider administering oxygen is responsible for monitoring the patient response and keeping the oxygen saturation levels within the target range. The most common reasons for initiating oxygen therapy include acute hypoxemia related to pneumonia, shock, asthma, heart failure, pulmonary embolus, myocardial infarction resulting in hypoxemia, post operative states, pneumonthorax, and abnormalities in the quality and quantity of hemoglobin. There are no contradictions to oxygen therapy if indications for therapy are present (Kane et al., 2013).
Hypoxic patients must be assessed for the causes and underlying reasons for their hypoxia. Hypoxia must be managed not only with supplemental oxygen but in conjunction with the interventions outlined in Table 5.3.
Table 5.3 Interventions to Treat and Prevent HypoxiaInterventionsAdditional Information
Raise the head of the bed Raising the head of the bed promotes effective breathing and diaphragmatic descent, maximizes inhalation, and decreases the work of breathing. Positioning enhances airway patency in all patients. A Fowler’s or semi-Fowler’s position promotes a patient’s chest expansion with the least amount of effort. Patients with COPD who are short of breath may gain relief by sitting with their back against a chair and rolling their head and shoulders forward or leaning over a bedside table while in bed. High Fowler’s position
Deep breathing and coughing techniques
Deep breathing and coughing techniques help patients effectively clear their airway while maintaining their oxygen levels. Teach patients “controlled coughing” by having them take a deep breath in and cough deeply with the mouth slightly open. If they have difficulty coughing, teach the huffing technique. This involves taking a medium breath and then making a sound like “ha” to push the air out fast with the mouth slightly open. This is done three or four times, and then
they are instructed to cough. If secretions are thick and tenacious, the patient may be dehydrated and require additional fluids (if medical condition does not contraindicate additional fluids).
Oxygen therapy and equipment
If patient is already on supplemental oxygen, ensure equipment is turned on and set the required flow rate and is connected to an oxygen supply source. If a portable tank is being used, check the oxygen level in the tank. Ensure the connecting oxygen tubing is not kinked, which could obstruct the flow of oxygen. Feel for the flow of oxygen from the exit ports on the oxygen equipment. In hospitals where medical air and oxygen are used, ensure patient is connected to the
oxygen flow port.
High Fowler’s position
Deep breathing and coughing techniques
Deep breathing and coughing techniques help patients effectively clear their airway while maintaining their oxygen levels. Teach patients “controlled coughing” by having them take a deep breath in and cough deeply with the mouth slightly open. If they have difficulty coughing, teach the huffing technique. This involves taking a medium breath and then making a sound like “ha” to push the air out fast with the mouth slightly open. This is done three or four times, and then
they are instructed to cough. If secretions are thick and tenacious, the patient may be dehydrated and require additional fluids (if medical condition does not contraindicate additional fluids).
Oxygen therapy and equipment
If patient is already on supplemental oxygen, ensure equipment is turned on and set the required flow rate and is connected to an oxygen supply source. If a portable tank is being used, check the oxygen level in the tank. Ensure the connecting oxygen tubing is not kinked, which could obstruct the flow of oxygen. Feel for the flow of oxygen from the exit ports on the oxygen equipment. In hospitals where medical air and oxygen are used, ensure patient is connected to the
oxygen flow port. Assess for underlying causes of the hypoxia. Is the potential problem respiratory or cardiovascular? What underlying respiratory or cardiovascular conditions exist? Complete respiratory and cardiovascular assessments may reveal potential abnormalities in these systems.
Obstructive sleep apnea Patients with obstructive sleep apnea (OSA) may be unable to maintain a patent airway. In OSA, nasopharyngeal abnormalities that cause narrowing of the upper airway produce repetitive airway obstruction during sleep, with the potential for periods of apnea and hypoxemia. Pressure can be delivered during the inspiratory and expiratory phases of the respiratory cycle by using a mask to maintain airway patency during sleep. The process requires consideration of each individual’s needs in order to to obtain compliance. Anxiety and depression The most common co-morbidities of COPD are anxiety and depression. Anxiety is related to chronic shortness of breath and an inability to breathe effectively. Anxiety and depression are chronically undertreated and may be relieved with breathing retraining, counselling, relaxation techniques, or anti-anxiety medications if appropriate. Data source: Cigna & Turner-Cigna, 2005; Kane et al., 2013; Maurer et al., 2008; Perry et al., 2007; Perry et al., 2014; Shackell & Gillespie, 2009Applying and Titrating Oxygen Therapy
When providing oxygen therapy, remember the following (Kane et al., 2013):
- Initiate oxygen according to hospital protocols when patients with respiratory or cardiovascular conditions warrant its use.Always assess for underlying respiratory diseases. Patients with COPD are risk for acute hypoventilation and carbon dioxide retention. Elevated CO2 levels increase risk for respiratory
failure or hyperventilation. With COPD patients, always check the physician orders for the required amount of oxygen and acceptable SaO2 range.Regardless of underlying conditions, your first priority should be to prevent or treat hypoxia. Never withhold oxygen for COPD patients while waiting for additional medical interventions (Alberta Health Services, 2015; British Thoracic Society, 2008).Check all equipment for safety and function least once per shift. Check
oxygen equipment more frequently if using a high-flow system, which requires higher oxygen concentration.Avoid interruption of oxygen therapy during patient transport.When patient has a tracheostomy or a high-flow oxygen system and is being transported out of your care, contact respiratory therapy for assistance.
Oxygen is available in hospitals through bulk liquid oxygen systems that dispense oxygen as a gas through outlets in rooms. It can also be provided in cylinders (large or small) for easy transport for patient use while mobile or when moving around the hospital. An oxygen flow meter regulates the flow in litres per minute. Oxygen therapy may be short- or long-term depending on the SaO2 requirements of the patients and underlying diseases processes (Perry et al., 2014).
Checklist 41 reviews the steps for applying and titrating oxygen therapy (see Figure 5.2).
Checklist 41: Applying and Titrating Oxygen TherapyDisclaimer: Always review and follow your hospital policy regarding this specific skill. Safety considerations:- Perform hand hygiene.Check room for additional precautions.
Introduce yourself to patient.Check patient’s name band to confirm identification. Explain process to patient.Use appropriate listening and questioning skills.Listen and attend to patient cues.Ensure patient’s privacy and dignity.Apply principles of asepsis and safety.
Assess for underlying medical conditions or alternate causes of hypoxia (cardiovascular).
2. If a patient requires oxygen therapy, choose an oxygen delivery system based on your patient’s requirements. Oxygen is initially started a low concentration (2 L/min) using nasal prongs. Then the flow is titrated up to maintain oxygen saturation of 92% or greater.Selection of delivery system is based on the level of oxygen support required (controlled or non-controlled), the severity of hypoxia, and the disease process. Other factors include age, presence of underlying disease (COPD), level of health, presence of an artificial airway, and environment (home or hospital).
Significant decreases to O2 saturation levels or large increases to maintain O2 saturation should be reported promptly to responsible health care provider.
3. Once oxygen is applied, reassess your patient in 5 minutes to determine the effects on the body toàn thân. Hypoxia should be reduced or prevented. O2 levels should be between 92% and 98%.Assess vital signs, respiratory and cardiovascular systems, and level of consciousness. Assess and implement additional treatments for hypoxia if appropriate.
Reassess your patient if signs and symptoms of hypoxia return.
4. If required, adjust O2 levels. Changes in O2 percentages should be in 5% to 10% increments.Patients should be reassessed (respiratory assessment including O2 saturations) after 5 minutes following any changes to oxygenation levels.
Changes in litre flow should be in 1 to 2 L increments.
Consider changing O2 delivery device if O2 saturation levels are not maintained in target range.
Slow, laboured breathing is a sign of respiratory failure.
5. If hypoxia continues, contact respiratory therapist or physician for further orders according to agency protocol. Patient may require further interventions from the respiratory therapist or most responsible health care provider.Signs and symptoms of respiratory deterioration include increased respiratory rate, increased requirement of supplemental oxygen, inability to maintain target saturation level, drowsiness, decrease in level of consciousness, headache, or tremors.
Data source: British Thoracic Society, 2008; Perry et al., 2014 Special considerations:- The underlying condition causing hypoxia must be treated to manage and improve patient outcomes. For example, if hypoxia is caused by pneumonia, additional treatment for hypoxia may include antibiotics, increased fluid intake, oral suctioning, position changes, and deep breathing and coughing exercises.If a patient has COPD, check physician order for the amount of required oxygen and the expected saturation level.
In general, COPD patients receive 1 to 2 L/min (Kane et al., 2013).Once oxygen saturation levels are within normal range, perform a respiratory assessment every two to four hours to monitor need for supplemental oxygen.When using oxygen therapy, assess the patient’s skin where the oxygen device comes into contact with the patient. The nose, chin, and ears may have skin breakdown due to the irritation of the tubing on the skin. Oxygen therapy tends to cause drying effects
to the nares and mouth. To prevent the drying effect, consider increasing fluid intake (if not contraindicated). Perform frequent mouth care and apply humidification if the patient is receiving more than 4 L/min (Perry et al., 2014).
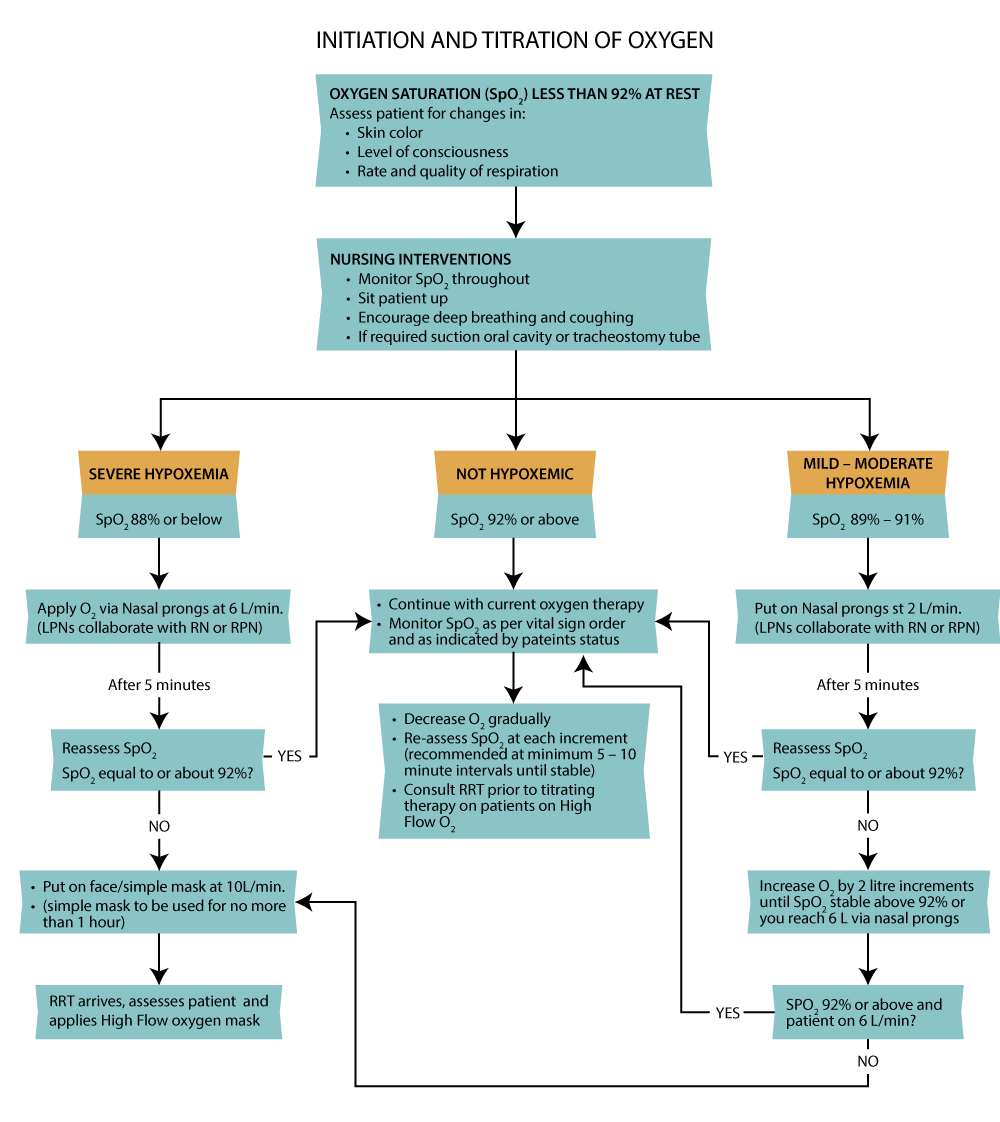 Figure 5.2 Oxygen therapy protocol (adapted from Providence Health Care, 2008)A patient is admitted with COPD and pneumonia and has an oxygen saturation of 88% on 1 L/min of oxygen. Is this an appropriate oxygenation level for a patient with COPD? Why?A patient with no underlying respiratory disease is hypoxic with an oxygen saturation level of 91% on room air. What are four additional interventions that may help improve
oxygen saturation levels without applying oxygen therapy?
Figure 5.2 Oxygen therapy protocol (adapted from Providence Health Care, 2008)A patient is admitted with COPD and pneumonia and has an oxygen saturation of 88% on 1 L/min of oxygen. Is this an appropriate oxygenation level for a patient with COPD? Why?A patient with no underlying respiratory disease is hypoxic with an oxygen saturation level of 91% on room air. What are four additional interventions that may help improve
oxygen saturation levels without applying oxygen therapy?
What are the priority nursing interventions for the patient while in the PACU?
Nursing interventions that are required in postoperative care include prompt pain control, assessment of the surgical site and drainage tubes, monitoring the rate and patency of IV fluids and IV access, and assessing the patient's level of sensation, circulation, and safety.What is the priority initial nursing assessment in the PACU?
When transferring care from PACU to the ward, patient identification and handover should occur utilising the Handover Flowsheet. Initial patient assessment should include: Physical Assessment of patient including Airway, Breathing, Circulation & Disability (Link to Nursing Assessment)What does a PACU nurse do?
PACU nurses are highly trained critical care nurses who work in a hospital's post anesthesia care unit (PACU). They care for patients who have just gotten out of surgery and are recovering from the effects of anesthesia.What is the main focus of care in post operative recovery room?
The practical nurse responsibility for the care of a patient in the recovery room is to prevent complications, detect early complications, relieve patient's discomfort, support patients through their state of dependence to independence, and closely monitor the patient's condition. Tải thêm tài liệu liên quan đến nội dung bài viết When a patient is admitted to the PACU what are the priority interventions the nurse performs